When most people think about breast cancer treatment, the first side effects that come to mind are hair loss, fatigue, or nausea. However, one often-overlooked area that can significantly affect daily life is the oral side effects of breast cancer treatment and how therapy impacts overall oral health.
Common oral complications include dry mouth, mouth sores, gum sensitivity, changes in taste, and an increased risk of infections. These breast cancer oral side effects can make eating, speaking, and even sleeping difficult, which in turn may affect nutrition, mood, and the ability to tolerate treatment.
This post discusses how cancer treatment affects dental health, highlights these lesser-known breast cancer oral side effects, and offers practical oral care tips for breast cancer patients. We will also explain how a compassionate dental practice, such as Dr. Christine Hansen’s in Palo Alto, CA, can be a supportive partner throughout every stage of treatment and recovery.
Why Oral Health Matters During Breast Cancer Treatment
The mouth is the gateway to the body. Oral problems during cancer treatment can:
- Interfere with nutrition by making eating painful or unpleasant.
- Increase the risk of infection—especially when the immune system is weakened—which can lead to greater dental decay and gum disease over time.
- Lower overall quality of life and disrupt treatment continuity.
A review published in the Journal of the International Society of Preventive & Community Dentistry found that women undergoing breast cancer therapy often experience gum inflammation, plaque accumulation, and oral burning sensations (PMC). Although these issues are common, they are often overlooked in oncology discussions. That’s why it’s critical to involve a dentist in your health care team—before, during, and after cancer therapy.
Patients in Palo Alto can rely on gentle dental care at Dr. Christine Hansen & Associates, where the team supports individuals through every stage of treatment and ensures oral health is closely managed alongside cancer care.
How Cancer Treatment Affects Dental Health
1. Chemotherapy
Chemotherapy drugs target rapidly dividing cells. While this is crucial for fighting cancer, it can also affect the rapidly dividing cells of the oral lining, leading to common side effects such as:
- Mouth sores (oral mucositis): Painful ulcerations or raw patches in the mouth. These can make eating and drinking extremely difficult (Cancer.gov).
- Weakened immunity: Lower white blood cell counts make patients more vulnerable to bacterial, viral, or fungal infections like oral thrush.
- Gum sensitivity & bleeding: Low platelet counts during chemotherapy can cause gums to bleed easily (Cancer Council).
- Dry mouth (xerostomia): Reduced saliva production increases the risk of cavities and discomfort (NIDCR).
- Altered taste (dysgeusia): Many patients notice metallic, bitter, or dull tastes that can diminish appetite (National Breast Cancer Foundation).
- Cavities: Without the protective role of saliva, tooth decay can progress rapidly.
Chemotherapy Mouth Care Tips
Practicing consistent chemotherapy mouth care can help ease discomfort and reduce complications:
- Brush gently 2–3 times a day using a soft-bristled toothbrush and mild fluoride toothpaste.
- Rinse frequently with a saltwater or baking soda solution (avoid alcohol-based mouthwashes).
- Stay hydrated to combat dry mouth—sip water throughout the day or use saliva substitutes recommended by your dentist.
- Avoid spicy, acidic, or rough foods that can irritate sores.
- Schedule regular dental visits before and during treatment to catch and manage issues early.
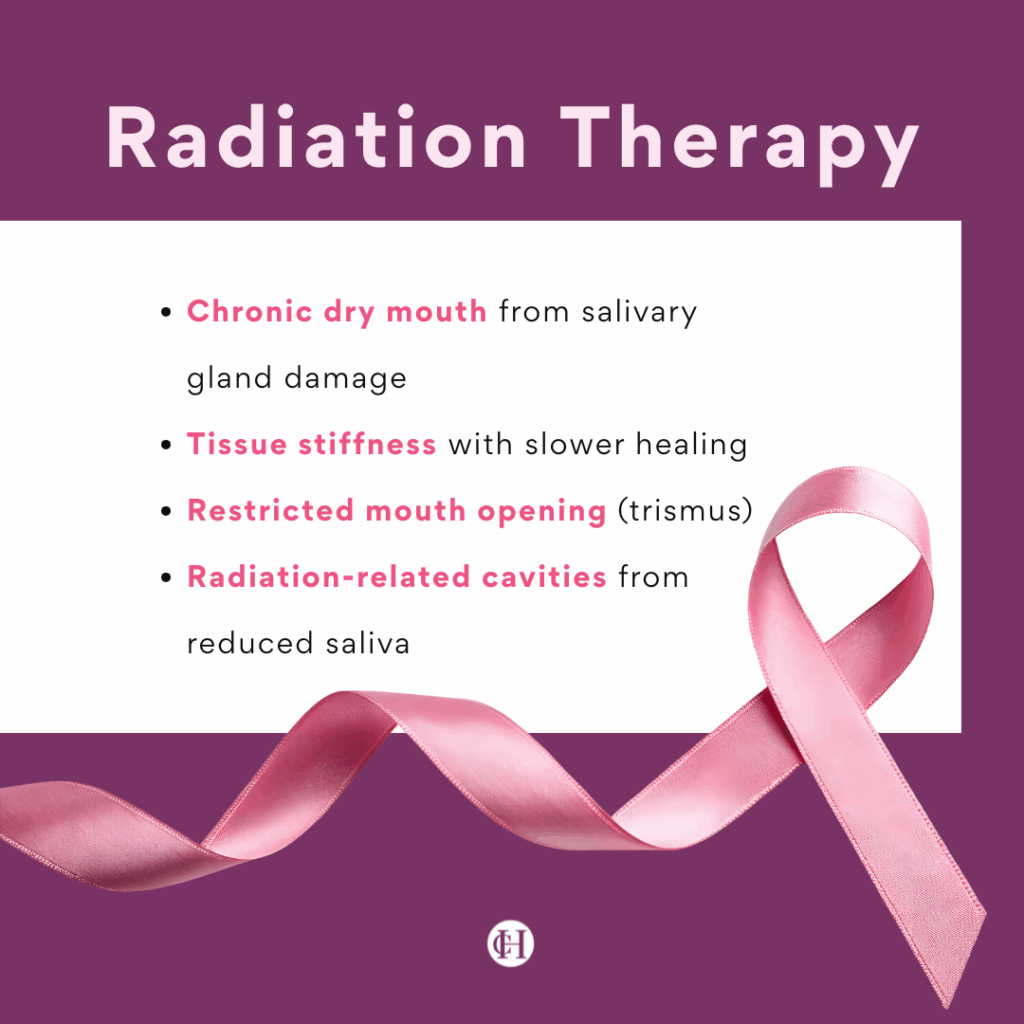
2. Radiation Therapy
Although breast cancer radiation is usually targeted to the chest, overlapping with the neck or jaw area in rare cases can lead to oral side effects, including:
- Persistent dry mouth resulting from salivary gland damage.
- Tissue stiffness and slower healing.
- Limited ability to open the mouth (trismus).
- Radiation-related cavities resulting from lasting saliva reduction (Brigham & Women’s Hospital).
3. Hormonal & Targeted Therapy
Aromatase inhibitors and tamoxifen can affect bone metabolism, which may indirectly influence gum and jaw health. Targeted therapies (like HER2 inhibitors) sometimes trigger oral irritation or mouth sores, especially when combined with chemotherapy (BreastCancer.org Podcast). Even without direct radiation to the head and neck, many breast cancer patients still face oral side effects from systemic treatments.
Common Oral Side Effects Patients Report
Some of the most frequently reported issues during cancer treatments—including chemotherapy, radiation, and targeted therapy—include:
- Dry mouth
- Painful sores and ulcers
- Gum swelling or bleeding
- Changes in taste
- Tooth decay and cavities
- Oral infections (thrush, cold sores)
- Jaw stiffness or soreness
While these problems may seem minor compared to fighting cancer itself, they can significantly impact comfort, nutrition, and recovery. Always talk to your doctor or nurse about any oral discomfort you experience during treatment, as early care can prevent complications. Simple daily habits—like brushing your teeth gently with a soft-bristled toothbrush and fluoride toothpaste—can go a long way toward protecting your mouth and easing discomfort throughout your care journey.
Oral Care Tips for Breast Cancer Patients
The good news: Many oral health issues that arise during breast cancer treatment can be managed or prevented with the right strategies.
Before Treatment Begins
- Schedule a Dental Exam: Visit your dentist at least 3–4 weeks before starting chemotherapy or radiation to address any existing problems (ADA).
- Get a Professional Cleaning: Consider starting fluoride treatments if recommended.
- Share Your Cancer Treatment Plan: Inform your dentist about your cancer diagnosis and treatment plan so they can coordinate care with your oncologist.
During Treatment
Daily Care
- Brush with a soft or ultra-soft toothbrush twice daily.
- Use mild or children’s toothpaste to avoid irritation.
- Floss gently each day, but pause if your platelet count is low to prevent gum bleeding or irritation.
- Rinse your mouth every 4–6 hours with a salt and baking soda solution or alcohol-free mouth rinses (MSKCC).
- Avoid alcohol-based mouthwashes.
- Stay hydrated and use sugar-free gum or lozenges to stimulate saliva.
- Ask your dentist about saliva substitutes or prescription stimulants if dryness is severe.
Eating Well
- Opt for soft, well-balanced foods such as soups, smoothies, and yogurt to maintain comfort and nutrition during treatment.
- Avoid spicy, acidic, or coarse foods that may aggravate oral tissues.
- Use a straw when needed to minimize contact with sore areas.
- Consume smaller, more frequent meals to support adequate nutrition.
Managing Pain & Infections
- Consult your dentist about prescription mouth rinses or topical gels to help relieve painful sores.
- Dentists may prescribe antifungal or antiviral medications if infections develop.
- Monitor blood counts before any dental procedure.
Fluoride Protection
- Use prescription-strength fluoride rinses or gels as recommended by your dentist.
- Consider custom fluoride trays if suggested.
- Reduce consumption of sugary snacks and beverages.
After Treatment
- If dry mouth persists, keep using fluoride treatments.
- Schedule dental cleanings more frequently (every 3–6 months).
- Stay vigilant for long-term side effects such as enamel erosion or gum recession.
- Notify your dentist about any ongoing cancer medications or hormone therapies.
When to Call Your Dentist Right Away
Seek dental care promptly if you notice:
- Severe or spreading mouth sores
- White patches (possible thrush)
- Difficulty swallowing
- Excessive gum bleeding
- Tooth pain or sensitivity
- Jaw pain or restricted opening
Catching problems early prevents them from escalating into serious infections or complications. Avoid spicy foods or anything that worsens irritation while waiting for professional care, and contact your provider immediately for guidance.
The Role of a Compassionate Dental Team
Your dentist is more than just someone who cleans teeth—they’re an essential partner in your overall health. At Dr. Christine Hansen and Associates in Palo Alto, CA, we:
- Coordinate with oncologists to ensure safe timing of dental procedures.
- Offer preventive care like fluoride treatments, gentle cleanings, and personalized hygiene plans.
- Provide comfort-focused options for patients with gum sensitivity or pain.
- Educate and support patients through every phase of treatment.
- Help survivors maintain oral health long after therapy ends.
Our goal is to help you maintain comfort, nutrition, and confidence so you can focus on healing.
Conclusion & Next Steps
Breast cancer treatment is a journey that affects the whole body, including oral health. Issues such as dry mouth, gum sensitivity, infections, and taste changes are common but manageable with the right strategies.
Key takeaways:
- Visit your dentist before treatment begins.
- Maintain gentle but consistent oral hygiene during therapy.
- Use rinses, fluoride, and saliva substitutes as needed.
- Stay alert for signs of infection or worsening sores.
- Partner with a compassionate dental team that understands your unique needs.
If you’re undergoing breast cancer treatment or are in recovery, don’t let oral side effects disrupt your health and comfort. Dr. Christine Hansen and Associates in Palo Alto, CA specializes in personalized, compassionate dental care for patients navigating complex medical conditions.
Contact our office today to schedule a consultation and take the first step toward protecting your oral health during your cancer journey.
